Quality Measures
Clinical excellence and patient safety are critical standards at Billings Clinic. One method used to measure our clinical excellence (also referred to as quality of care), is by comparing our performance to state and national patient quality benchmarks.
Billings Clinic strives to effectively use proven methods to improve every aspect of care for all of our patients and measure our performance in many areas. Below are some of the key metrics we monitor to demonstrate our dedication to clinical excellence and patient safety.
Quality Measures
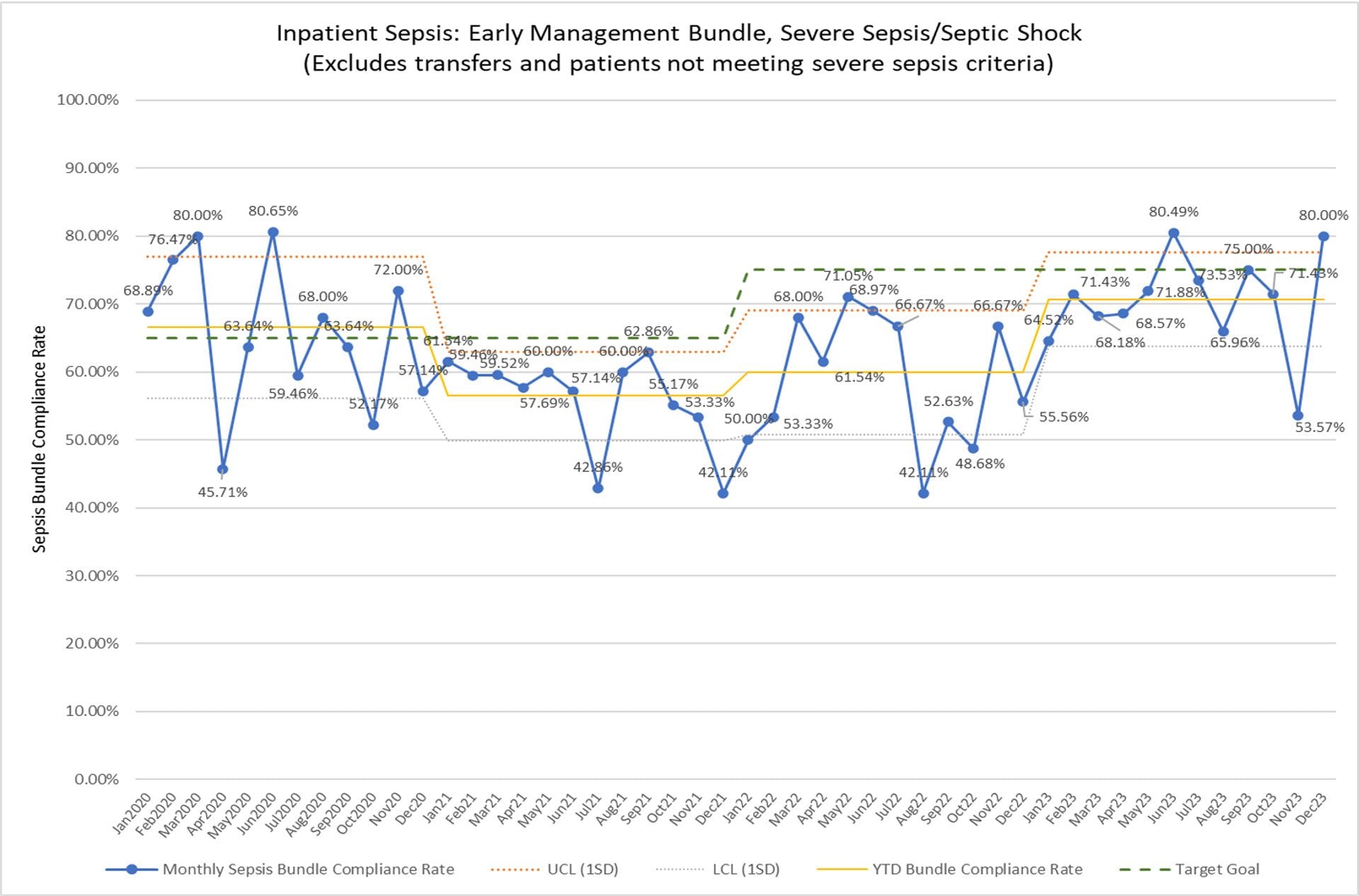
Sepsis Bundle
Initial response for sepsis and septic shock designed to minimize time to treatment.
- Critical labs performed by nurses at the bedside in the Emergency Department.
- Standardized orders created to support best practice in sepsis care.
- Concurrent review of all hospital sepsis patients and real-time feedback provided to physicians and APPs to support learning.
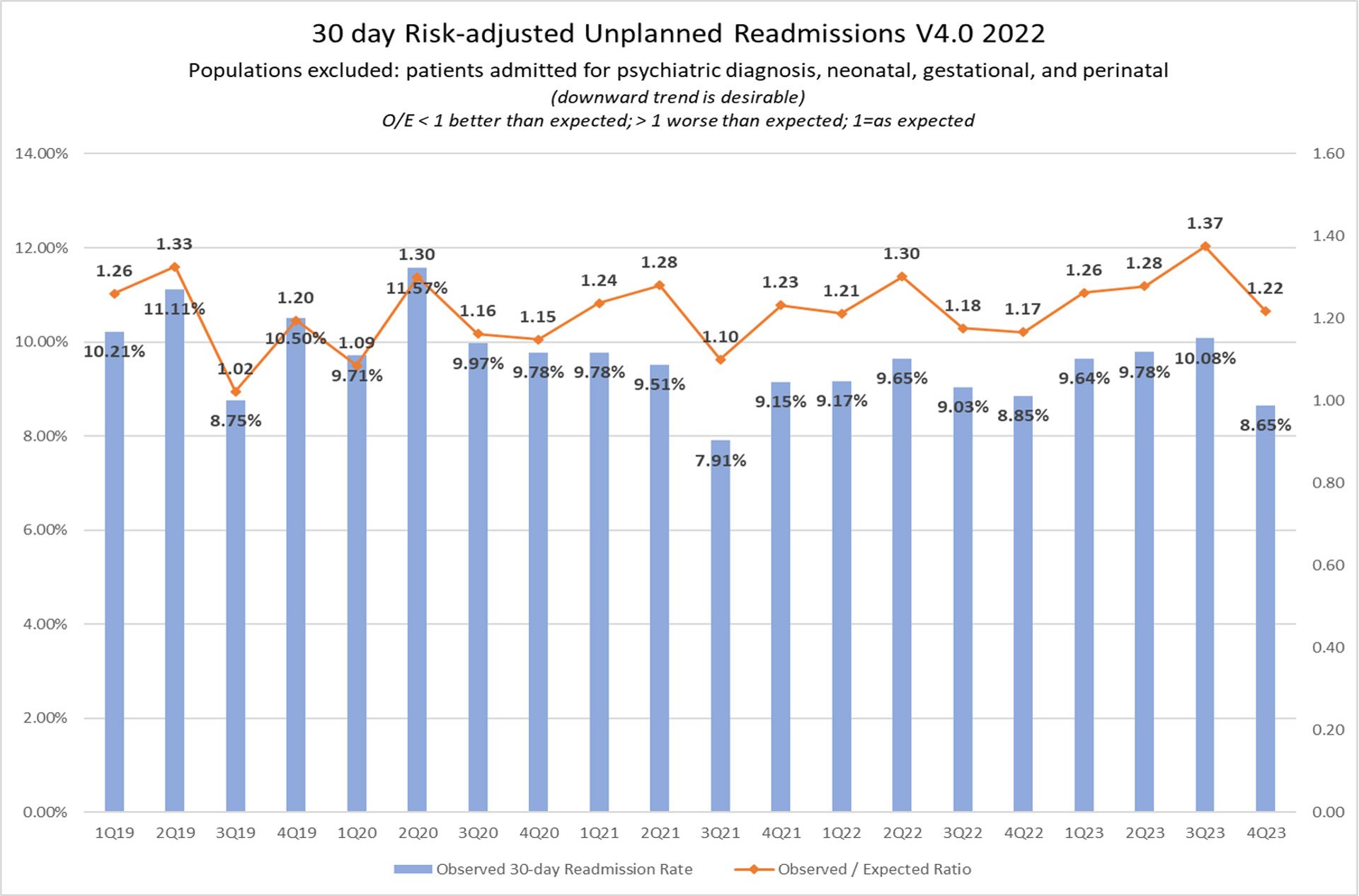
Readmissions
Billings Clinic tracks patients who experience an unplanned readmission to the hospital within 30 days after a previous hospital stay. The readmission to the hospital can be for any reason, not necessarily associated with the previous hospital stay. Improvement work includes multidisciplinary discharge rounds, cross-functional learning with focused populations like COPD, heart failure, stroke, heart attack and hip/knee replacement patients.
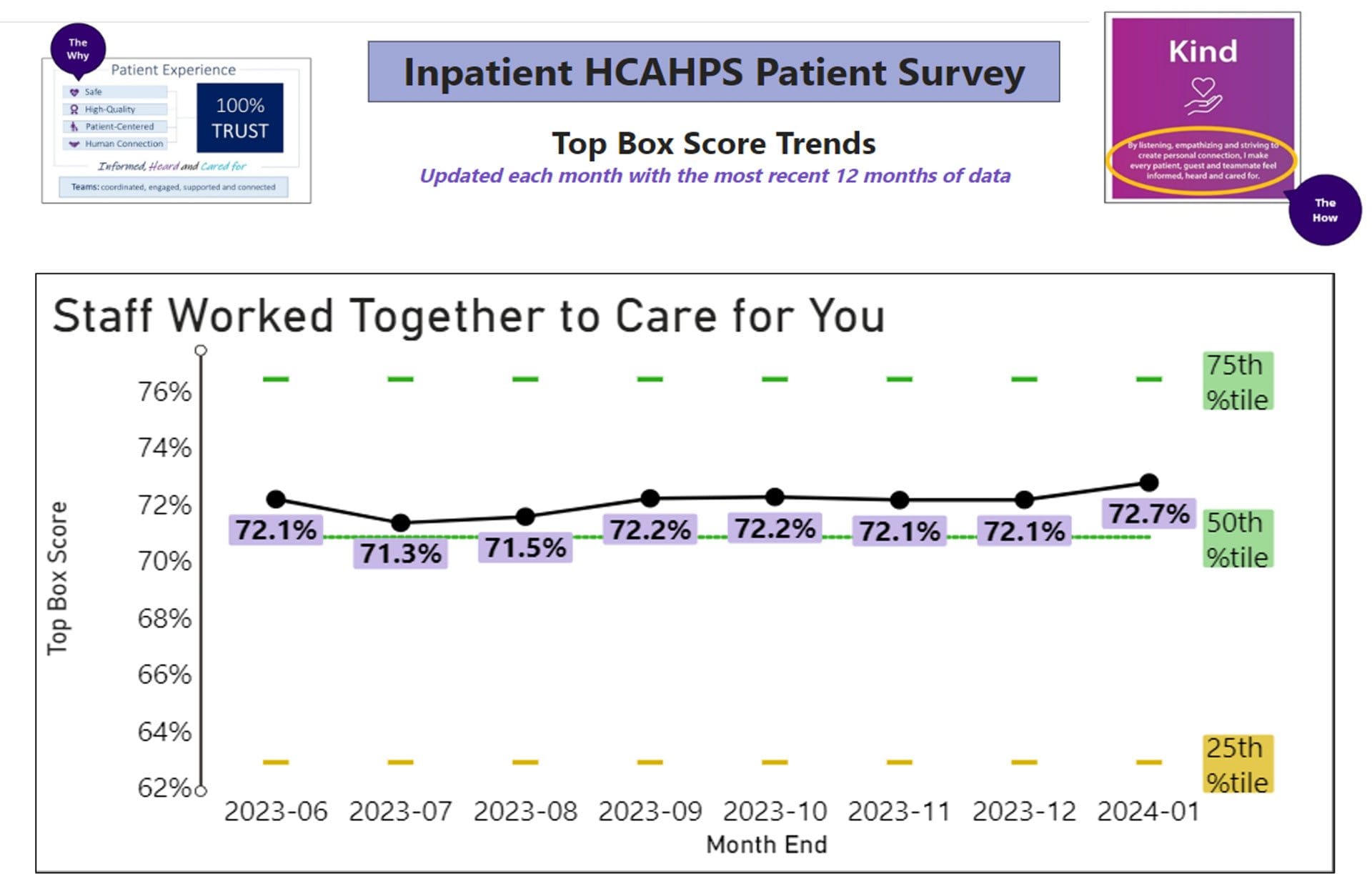
Patient Experience
We strive to make everyone that comes to Billings Clinic feel informed, heard and cared for. One of the tools used to measure this is HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) surveys. The following graph is a visualization of “Staff Worked Together to Care for You”. This is an overall assessment question that is representative of a variety of aspects of patient experience including communication, education, and coordination.
Involving Patients in Prevention
5 Things Patients Can Do to Prevent Infections
- Clean their hands. Watch their healthcare providers and visitors and remind them to wash their hands before entering the room.
- Pay attention to changes in their body. Informing their care providers if they notice signs and symptoms of infection (e.g., redness or swelling near an IV site).
- Take antibiotics only when needed. Take antibiotics only as directed.
- Remember to schedule your annual exam. Talk to your provider and stay up to date on all recommended vaccinations (e.g., influenza, pneumococcal, shingles, COVID-19, RSV).
- Speak up and ask questions. Tell their providers about any concern or information about their health. The more providers know, the more they can help patients stay well.
Health Care-Associated Infections (HAI) Prevention Measures
Clostridioides difficile (C. diff) intestinal infections
- Initiate Special Contact Precautions promptly for diarrhea
- Maintain Special Contact Precautions throughout duration of hospitalization if C. diff is confirmed
- Perform hand hygiene with soap and water for 20 seconds
- Disinfect high touch surfaces and patient environment
- Disinfect medical equipment after use with bleach based cleaner
- Ensure daily patient bathing or showering with soap and water
- If C diff positive, do not repeat testing as patients may remain positive for ≥6 weeks
Catheter-associated urinary tract infections (CAUTI)
INSERTION:
- Insert only when absolutely needed – Consider external devices or intermittent catheters
- Perform excellent hand hygiene and use superb sterile technique for insertion
- Utilize two people to maintain sterile procedure
MAINTENANCE:
- Maintain a closed system
- Remember peri care every shift and as needed
- Keep catheter stable and below bladder to ensure drainage
REMOVAL:
- Remove catheter as soon as possible
No catheter is the best catheter
Central line-associated bloodstream infections (CLABSI)
The nation witnessed an increase in CLABSI through the SarS-CoV-2 pandemic and Billings Clinic also saw an increase in the CLABSI rate through 2021. Recognizing the increased patient harm and cost associated with this healthcare-associated infection, we formed a multidisciplinary group of individuals to rapidly implement evidence-based improvements from decision for placement to removal of the central line. Some of the improvements are below:
INSERTION:
- Create pre-line insertion flow chart with roles and responsibilities
- Emphasize checklist utilization, catheter type and insertion location
- Ensure lines placed outside Billings Clinic are replaced, when possible, once in the intensive care unit
MAINTENANCE:
- Refocus efforts at daily CHG (chlorhexidine gluconate) bathing for patients with central lines
- Implement Scrub the Hub program for all central lines prior to accessing for medication or fluid administration
- Investigate update necessity of current central line dressing kit in collaboration with supply chain
REMOVAL:
- Utilize multidisciplinary rounds as a required daily discussion on necessity of central line in order to remove central lines as soon as safely possible
Surgical Site Infections
- Implement perioperative glycemic control and use blood glucose targets less than 200 mg/dL in patients with and without diabetes
- Maintain perioperative normothermia
- Advise patients to shower or bathe (full body) with an antiseptic agent on at least the night before the operative day
- Perform intraoperative skin preparation with an antiseptic agent unless contraindicated
- Hair removal should be avoided unless hair interferes with surgery. If hair removal is necessary, clippers should be used instead of a razor
- Use of a waterless chlorhexidine scrub is as effective as traditional water scrub and requires less time
- Smoking cessation 4-6 weeks before surgery reduces SSI and is recommended for all current smokers, especially those undergoing procedures with implanted materials
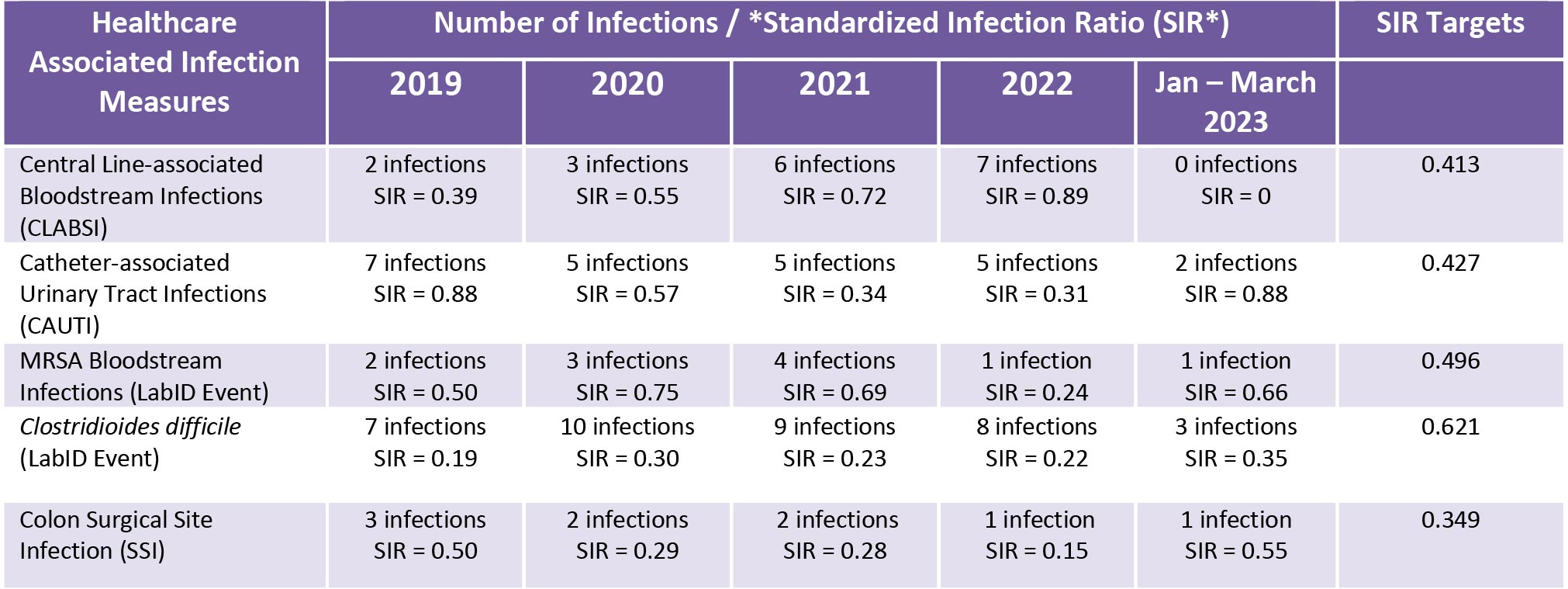
*Standardized Infection Ration (SIR) is the risk adjusted metric used by the Centers for the Disease Control’s National Healthcare Safety Network for reporting of Healthcare-associated Infections.